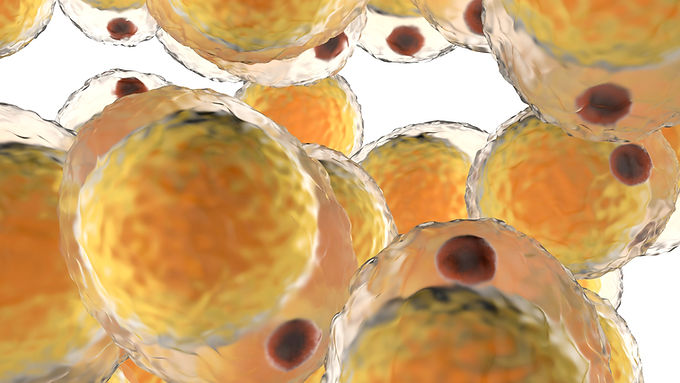
A recent randomized controlled trial (RCT) in the European Journal of Clinical Nutrition (EJCN) showed that those consuming a high carbohydrate diet (60% carbohydrate as a proportion of total energy, n = 10) had lower rates of maximal adipose tissue mitochondrial respiration than those consuming a moderate carbohydrate diet (40%, n = 8, p = 0.039) or a low carbohydrate diet (20%, n = 9, p = 0.005) after 10 to 15 weeks. The study looked at whether adipocyte mitochondrial respiration may influence metabolic fuel partitioning into oxidation versus storage, with implications for whole-body energy expenditure. The authors explain that this preliminary finding may provide a mechanism for postulated calorie-independent effects of dietary composition on energy expenditure and fat deposition, potentially through the actions of insulin on fuel partitioning.
The question of whether dietary macronutrient composition affects energy balance is an ongoing and hotly debated topic, and the authors explain that although insulin has been shown in the literature to influence mitochondrial respiration, the effects of dietary macronutrient composition have not been well characterized, therefore, the goal of their study was was to test the hypothesis that a high-carbohydrate diet lowers the oxygen flux of adipocyte mitochondria ex vivo (outside the body). Though it was shown that a high carbohydrate diet alters mitochondrial capacity for energy production in fat tissue, no clear evidence was provided in this exploratory paper on whether increased insulin secretion was a mechanism for the effects that were found from consumption of a high carbohydrate diet on adipose tissue mitochondrial respiration (insulin was not measured), though there are clues that indicate it is not just the amount of calories we consume, but the quality of those calories may matter more.
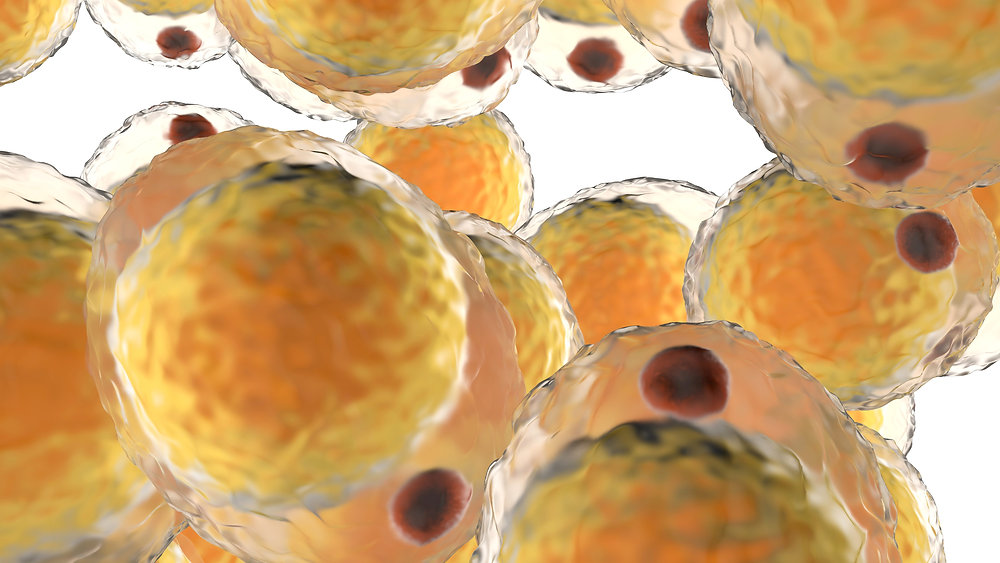
Adipose tissue, or fat tissue, is often seen as a passive storage unit. Yet, it is actually a complex and vital part of our endocrine system, involved in maintaining our energy balance and mediating our responses to nutrients. The impact of diet on these functions, particularly a diet high in carbohydrates, is a topic of research and debate. In this blog post, we will delve deep into the biochemical mechanisms behind why a high carbohydrate diet can impair the mitochondrial function in fat cells, potentially predisposing us to obesity.
However, let's look at the biochemical impact of a high carbohydrate diet on adipose tissue outside the paper, and try to unravel the mitochondrial conundrum.
A Carbohydrate-Heavy Diet: Affecting Mitochondrial Capacity
To begin, let’s understand the role of carbohydrates in our body. They are the primary source of energy, which are broken down into glucose that enters our cells and is metabolically converted into ATP, the cellular currency of energy. This process is facilitated by insulin, which is secreted in response to elevated blood glucose levels.
Now, let’s turn our attention to our fat cells, or adipocytes, where much of this glucose is destined. The first step in processing glucose within these cells is its conversion to glucose-6-phosphate (G6P) by the enzyme hexokinase. This is akin to a gatekeeper allowing entry to a specific guest, in this case, glucose, into the cell.
Once inside, G6P can follow a couple of pathways. It can go through glycolysis, producing pyruvate which then enters the mitochondria and becomes a part of the citric acid cycle (TCA cycle), or it can be converted into glycerol-3-phosphate, which is used for the synthesis of triglycerides, a storage form of fat. This decision is like a traffic light system where the abundance of glucose decides the direction of traffic.
When our diet is high in carbohydrates, there’s an overabundance of glucose, leading to an accumulation of G6P. This excess G6P inhibits hexokinase, leading to an increase in intracellular glucose concentrations. On the other hand, it promotes the conversion of G6P to glycerol-3-phosphate, favoring fat storage over energy production. This is like a city dealing with excess traffic by routing cars into a parking lot instead of allowing them to flow onto the highway.
High Carbohydrate Diet and Impaired Mitochondrial Respiration
But what about mitochondrial respiration? As mentioned earlier, when glucose is abundantly available, it is preferentially stored as fat, and fewer molecules of pyruvate enter the TCA cycle. This reduction in pyruvate supply leads to decreased flux through the TCA cycle and electron transport chain, ultimately reducing mitochondrial ATP production. It’s like a power plant operating at a lower capacity because the fuel supply (in this case, pyruvate) is scarce.
Insulin: A Potential Mediator
Now let's discuss the role of insulin in this process. A high carbohydrate diet leads to increased insulin secretion. Insulin, among its many functions, inhibits the hormone-sensitive lipase enzyme, which is responsible for breaking down stored fats (triglycerides) into free fatty acids that can be used for energy. This is like insulin putting a lock on the fat storage, making it difficult for our body to access it when needed.
The constant presence of insulin from a high carbohydrate diet not only promotes fat storage but also discourages fat breakdown and usage. This insulin-dominant environment, therefore, represses the normal cycle of fat deposition and mobilization, leading to an overall increase in adiposity.
Carbohydrate-Insulin Model (CIM) Vs. Energy Balance Model
Which brings us to the two prevailing models of obesity – the Carbohydrate-Insulin Model (CIM) and the Energy Balance Model.
The Energy Balance Model (EBM) proposes that weight gain is simply a matter of consuming more calories than we burn. However, this model does not account for the different metabolic and hormonal responses elicited by different macronutrients.
On the other hand, CIM argues that the quality of calories matters. It suggests that a diet high in carbohydrates, especially refined carbohydrates, leads to a hormonal cascade, initiated by insulin, that promotes fat storage and inhibits fat mobilization, predisposing individuals to weight gain and obesity.
From the paper above to my applied clinical experience in all levels of obesity, I lean toward the CIM, as just like fueling a car with high-quality fuel leads to better performance, feeding our body with the right kind of nutrients affects our metabolic performance and body weight.
In conclusion, a diet high in carbohydrates may have a profound impact on mitochondrial energy production in adipocytes and potentially drive an increased risk of obesity, though future research is needed, and should focus on identifying the pathways and mechanisms of action to provide better treatment options for those struggling with obesity.
Link: https://www.nature.com/articles/s41430-022-01097-3
Yours in Health,

Dr. Steven Finch, DHSc, MHA, MSACN, MS, CNS, LDN, RCEP, CSOWM, CSCS
Lifestyle Evolution
Integrative/Functional Weight Loss Health Coach